From the CDC….
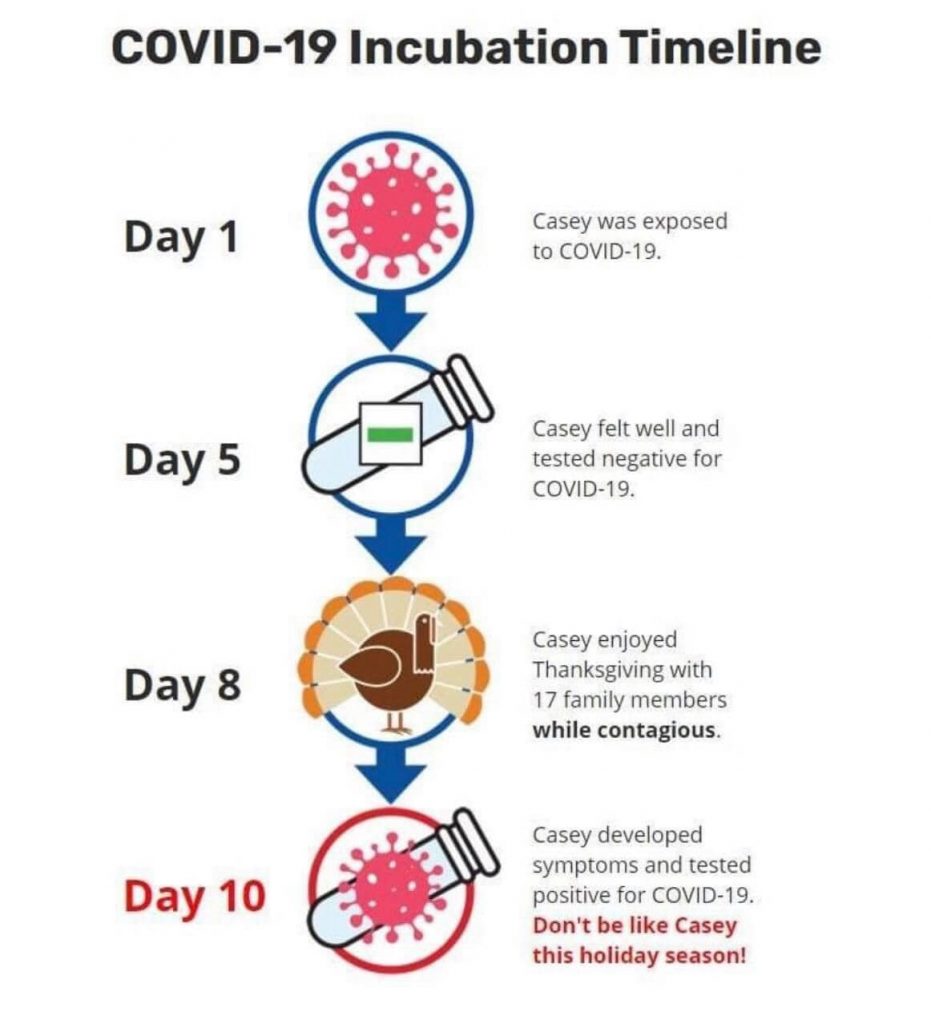
Incubation period
The incubation period for COVID-19 is thought to extend to 14 days, with a median time of 4-5 days from exposure to symptoms onset.(1-3) One study reported that 97.5% of people with COVID-19 who have symptoms will do so within 11.5 days of SARS-CoV-2 infection.(3)
Presentation
The signs and symptoms of COVID-19 present at illness onset vary, but over the course of the disease many people with COVID-19 will experience the following:(1,4-9)
- Fever or chills
- Cough
- Shortness of breath or difficulty breathing
- Fatigue
- Muscle or body aches
- Headache
- New loss of taste or smell
- Sore throat
- Congestion or runny nose
- Nausea or vomiting
- Diarrhea
Symptoms may differ with severity of disease. For example, shortness of breath is more commonly reported among people who are hospitalized with COVID-19 than among people with milder disease (non-hospitalized patients).(10, 11) Atypical presentations of COVID-19 occur often, and older adults and people with medical comorbidities may experience fever and respiratory symptoms later during the course of illness than people who are younger or who do not have comorbidities.(12, 13) In one study of 1,099 hospitalized patients, fever was present in only 44% at hospital admission but eventually 89% of patients had a fever sometime during hospitalization.(1) Fatigue, headache, and muscle aches (myalgia) are among the most commonly reported symptoms in people who are not hospitalized, and sore throat and nasal congestion or runny nose (rhinorrhea) also may be prominent symptoms. Many people with COVID-19 experience gastrointestinal symptoms such as nausea, vomiting or diarrhea, sometimes prior to having fever and lower respiratory tract signs and symptoms.(9) Loss of smell (anosmia) or taste (ageusia) has been commonly reported, in a third of patients in one study, especially among women and younger or middle-aged patients.(14)
Asymptomatic and Presymptomatic Infection
Several studies have documented infection with SARS-CoV-2, the virus causing COVID-19, in patients who never have symptoms (asymptomatic) and in patients not yet symptomatic (presymptomatic).(15-29) Since people who are asymptomatic are not always tested, the prevalence of asymptomatic infection and detection of presymptomatic infection is not yet well understood. Current data, based on reverse transcription-polymerase chain reaction (RT-PCR) testing for SARS-CoV-2 and on serologic studies, suggest asymptomatic infections can be common and that the total number of infections is likely greater than the number of cases reported.(15,22-24,30,31) Patients may have abnormalities on chest imaging before the onset of symptoms.(16)
Asymptomatic and Presymptomatic Transmission
Increasing numbers of epidemiologic studies have documented SARS-CoV-2 transmission during the presymptomatic incubation period.(19,28,29,32) Studies using RT-PCR detection have reported low cycle thresholds, indicating larger quantities of viral RNA, among people with asymptomatic and presymptomatic SARS-CoV-2 infection. Likewise in viral culture, viral growth has been observed in specimens obtained from patients with asymptomatic and presymptomatic infection.(22,24,27,33) The proportion of SARS-CoV-2 transmission due to asymptomatic or presymptomatic infection compared with symptomatic infection is not entirely clear; however, recent studies do suggest that people who are not showing symptoms may transmit the virus.(22,24,34)
Clinical Course
Illness Severity
The largest cohort reported to date, including more than 44,000 people with COVID-19 from China, showed that illness severity can range from mild to critical:(35)
- Mild to moderate (mild symptoms up to mild pneumonia): 81%
- Severe (dyspnea, hypoxia, or more than 50% lung involvement on imaging): 14%
- Critical (respiratory failure, shock, or multiorgan system dysfunction): 5%
In this study, all deaths occurred among patients with critical illness, and the overall case fatality ratio (CFR) was 2.3%.(35) The CFR among patients with critical disease was 49%.(35) Among children in China, illness severity was lower than in adults, with 94% of affected children having asymptomatic, mild, or moderate disease; 5% having severe disease; and less than 1% having critical disease.(13) Among U.S. COVID-19 cases reported January 22–May 30, 2020, overall the proportion of people who were hospitalized was 14%, including 2% admitted to the intensive care unit (ICU). Overall 5% of patients died.(36)
Clinical Progression
Among patients in multiple early studies from Wuhan, China who had severe COVID-19 illness, the median time from their onset of illness to the time they experienced dyspnea was 5–8 days; the median time from onset of illness to acute respiratory distress syndrome (ARDS) was 8–12 days; and the median time from onset of illness to ICU admission was 9.5–12 days.(5,6,37,38) Clinicians should be aware of the potential for some patients with COVID-19 to rapidly deteriorate about one week after illness onset. Among all hospitalized patients, 26%–32% of patients were admitted to the ICU.(6,8,38) Among all patients, 3%–17% had ARDS compared with 20%–42% for hospitalized patients and 67%–85% for patients admitted to the ICU.(1,4-6,8,38) Mortality among patients admitted to the ICU ranged from 39% to 72% depending on the study and characteristics of patient population.(5,8,37,38) The median length of hospitalization among survivors was 10–13 days.(1,6,8)
Risk Factors for Severe Illness
Age is a strong risk factor for severe illness, complications, and death.(1,6,8,13,34,35,39-42) Among the cohort of more than 44,000 confirmed cases of COVID-19 in China, the CFR increased with advancing age, and was highest among the oldest cohort. Mortality among people 80 years and older was 14.8%; 70–79 years, 8.0%; 60–69 years, 3.6%; 50–59 years, 1.3%; 40–49 years, 0.4%; and for those younger than 40 years, 0.2%.(35) Based on U.S. epidemiologic data through March 16, 2020, CFR was highest in people aged 85 years or older (range 10%–27%), followed by people aged 65–84 years (3%–11%), aged 55–64 years (1%–3%), and was lower in people younger than 55 years (<1%).(39)
CFR in the large cohort in China was elevated for patients with comorbidities, with 10.5% of those with underlying cardiovascular disease, 7.3% of those with diabetes, 6.3% of those with chronic respiratory disease, and 5.6% of those with cancer dying of COVID-related illness.(35) Prior stroke, diabetes, chronic lung disease, and chronic kidney disease have all been associated with increased illness severity and adverse outcomes due to COVID-19. Heart conditions, including heart failure, coronary artery disease, cardiomyopathies, and pulmonary hypertension, put people at higher risk for severe illness from COVID-19. People with hypertension may be at an increased risk for severe illness from COVID-19 and should continue to take their medications as prescribed. (43)
Accounting for differences in age and prevalence of underlying conditions, the mortality associated with COVID-19 that has been reported in the United States appears similar to reports from China.(36, 39) See People Who Are at Increased Risk for Severe Illness to learn more about who is at increased risk.
Reinfection
To date, limited data exist about reinfection with SARS-CoV-2 after recovery from COVID-19.(44-46) Published case reports have shown that reinfection is possible, but it is still unclear how long people who have recovered from COVID-19 are protected against reinfection with SARS-CoV-2, what concentration of antibodies is needed to confer protection, and how often reinfection may occur.(44-46)
While viral RNA shedding declines with resolution of symptoms, SARS-CoV-2 RNA shedding may continue for days to weeks.(37,47,48) Thus, detection of viral RNA during convalescence does not necessarily indicate replication-competent virus (infectiousness) or the presence of new infectious virus. Clinical infection has been correlated with the detection of IgM and IgG antibodies.(48-51) People who have recovered can continue to shed detectable SARS-CoV-2 RNA in upper respiratory specimens for up to 3 months after illness onset, albeit at concentrations considerably lower than during illness, in ranges where replication-competent virus has not been reliably recovered and infectiousness is unlikely. For more information about duration of viral shedding among people with SARS-CoV-2 infection, see Duration of Isolation and Precautions for Adults with COVID-19. Also see CDC’s Investigative Criteria for Suspected Cases of SARS-CoV-2 Reinfection as well as the Common Investigation Protocol for Investigating Suspected SARS-CoV-2 Reinfection.






 EastTexasRadio.com Powered by Ten Stations
EastTexasRadio.com Powered by Ten Stations